President's Message: Paul H. Earley, MD, DFASAM, Winter 2018
Saturday, December 1, 2018
World in Changes1
Paul H. Earley, MD, DFASAM
Change is accelerating. We can feel it in almost every sphere of human endeavor. Some areas are accelerating faster than we can imagine, even if we try very hard to do so (e.g., artificial intelligence), and some are just changing whether we like it or not (e.g., medicine). All are changing. Speaking personally, I have aged to the point where I regularly fall back into lamenting “the good old days” when considering many human endeavors, but none more so than medicine. Don’t get me wrong, I do not prefer the crude rendition of a plain film of my knee to the detail of an MRI. What I miss are the times when my internist actually knew my medical history and communicated it to my specialist via a formal letter. Now I show up for an appointment and the specialist asks, “Why exactly are you here?”
The Physician World
The art and practice of medicine have changed dramatically during my lifetime. The art of a thorough exam followed by a differential diagnosis seems to be lost. Medical technology has rendered many such skills unnecessary and therefore obsolete. Medical records are shared electronically, so, in theory, any specialist I see has my records instantaneously (more on this in a moment). And by the way, the more things change, the faster they change. Take a look at this reference2 in the endnotes for a great explanation.
Much of the change affects our participants. The number of physicians working in private practice decreased to 33 percent by the end of 2016, down from 57 percent sixteen years previously.3 In a study by Accenture, 92 percent of physicians chose employment out of necessity. Almost half of physicians reported they will look to sell their private practices within ten years.4 The list goes on and on. Physicians in training look at me as if I am from Mars when I foolishly ask: “Are you thinking about private practice?” This is not to say private practice is a panacea. But during the transition from a system of independent practitioners to corporate medicine, much strife occurs. Many participants in my PHP discuss their monthly visits with corporate “efficiency experts” to help them cut costs and work faster.
A second change we all bemoan is the electronic medical record. In full disclosure, I am a computer geek of the strongest sort. In the 1990s I built a company that produced one of the first electronic medical records for psychiatry and addiction treatment. This journey taught me that the problem is not the computer. The problem lies in how the EMR is coded and implemented.
The practice of medicine is complex and often nebulous; the path through a patient visit is not predictable. Conclusions about a case are often hard to distill down to an essential core—especially when the computer screen is staring you in the face asking for information that does not have anything to do with what is happening in the examination room. The computer’s demand for unneeded and irrelevant information, backed by patient care standards that demand completion of multiple screenfuls of irrelevant data, further reduces the physician’s sense of autonomy and relevance in saving lives. Such problems can be solved only by applying deep thought to the human–computer interface. This, I predict, will not occur in our lifetime.
A third change is in the delivery system itself. In our lifetime medical care has exploded and is using more expensive testing and equipment and we have a deeper understanding of thousands of disease states with more effective but costly procedural and surgical interventions. Entire subsectors of medical care were constructed, including the one many of us have worked in: addiction medicine. A new term came to the fore in medicine: cost containment—a phrase my father as a surgeon from a previous era never uttered. Third-party payors became vigilant, even indignant, about real and perceived unnecessary and at times fraudulent charges. The tension between practitioner and payer deepened and distressed us all.
We add to these three items a fourth factor: physician personality. I have had the pleasure of working with fine psychologists over the years who repeatedly point out to me that physicians have a surfeit of compulsivity. In fact, compulsive personality traits are normative. In a classic article,5 Gabbard points out that doubt, guilt feelings, and an exaggerated sense of responsibility form a compulsive triad in the personality of the physician. These are the very same characteristics that collide with a loss of autonomy that is commonly part of becoming employed. This collision is especially problematic for physicians of our generation, who have moved from independent practitioners to employees. External drivers that pressure us to work harder and see more patients are not needed in most cases and only serve to exacerbate the physician’s harsh internal critic. This characteristic is stressed to the breaking point when the EMR asks for pages upon pages of information unrelated to the care of each patient of the bucketloads seen in clinic. The dedicated, dutiful physician works long into the night to complete medical records of too many patients crammed into the daylight hours. Physicians who are trained to be independent thinkers often find themselves compressed into a box by EMRs and corporate structures, well-meaning or not.
PHPs witness the final result. Crumbling marriages, burnout, depression, and suicide are the result. It is no coincidence that the hottest current topic in physician health is burnout. The word is on the lips of every concerned leader in organizational medicine. The Maslach Burnout Inventory, pioneered in 1981 by Maslach and Jackson,6 has become one of the most talked about instruments in social science—for a second time. New conferences on physician health have emerged with a primary focus on job-related stress and the systemic dysfunction it produces.
Physician suicide (arguably, in some cases, a partial consequence of unfettered workplace dysfunction) has been the subject of several feature articles in major newspapers. A fine meta-analysis by Schernhammer showed the suicide ratio for male physicians was 1.41 when compared with the general population. For female physicians, this ratio is a whopping 2.27.7
Lesser markers of stress also abound. The divorce rate among physicians is quite high and seems to be correlated to specialty. The divorce rate for psychiatrists is 51 percent, 33 percent for surgeons, 24 percent for internists, 22 percent for pediatricians and pathologists, and 31 percent for other specialties.8 Nonetheless, it is important to remember that such percentages only underscore the extent of the problem and do not impute causation.
Taken together, this means PHPs are more relevant now than we have ever been in our history. We need to change, to become more efficient, to develop standards that improve what we do—while working under significant pressure and budgetary constraints.
The PHP World
In a similar way, PHPs and the FSPHP are in their own world of changes. Early PHPs were constructed de novo, and protocols for participant flow, monitoring, and oversight were unique products erupting out of the minds of each PHP pioneer. Soon directors and staff gathered together to discuss cases and procedures and to compare notes on process and procedures. Despite being unified by a desire to help our participants, each PHP felt unique. An oft-heard trope was, “When you have seen one PHP, you have seen one PHP.”
Soon after being established, the FSPHP subtly shifted the winds. Formed in 1990, the FSPHP evolved rapidly, and our annual meetings and committees increased discussions between states. Each PHP remained unique; however, best practices evolved out of our desire to do better. Many members brought their research and academic interests to the table. PHP research was born.
Discussions in our committees led to standards9 that pushed us all to greater conformity.
PHPs are disease-monitoring systems, not treatment, per se. Nonetheless, like all of medicine, we are subject to pressures to standardize protocols. We have a distinct advantage to most behavioral health programs in that we have both expert consensus protocols and outcome data that support the efficacy of those protocols. Still we have naysayers. Any system that grows to a certain size has its disgruntled participants and critical observers. Some appear articulate, especially to those who do not comprehend the importance of protecting the public and thus asking much of our participants.
Public safety is complex in and of itself. The press, interest groups, and the public at large have vast and untethered notions about the dangers that could potentially emerge when a medical professional develops a mental health problem. In the real world such dangers are rare, especially when compared to the negative outcomes that result from sleep deprivation, overwork, and poor communication among hospital staff. Thus, we are unceremoniously plopped into the business of managing public opinion. And no opinion is more important (and at times fickle) than that of our medical boards. Any one of our external stakeholders has the potential to construct standards out of their own idiosyncratic notion of what makes up a PHP.
All this has led to an inexorable conclusion. Both positive forces (our science-based interest in best practices, increased communication between PHPs, our creation of an effective parent—the FSPHP—and well-meaning external stakeholders) and negative forces (uninformed and not-so-well-meaning external pressure and the vicissitudes of political bodies) have come together to help us evolve. If we fail to build our own standards, we run the real risk of external organizations forcing less informed practices on us. The time to act is now.
The good news is that we are up to the task. The Accountability, Consistency, and Excellence (ACE) Committee is deep into rewriting best practice protocols and standards for PHPs. The FSPHP has contracted with Metacred, an Association Management Company (AMC) that specializes exclusively in credentialing.10 They will work hand-in-hand with the FSPHP to build two review systems.
The first is the Performance Enhancement and Effectiveness Review (PEER™) Program for our member PHPs. We will operationalize the standards set forth by the ACE Committee into a review that will catalog the accomplishments of each PHP and at the same time provide a road map to enhance growth and quality. Some of our member PHPs have already undergone external review, looking to document their successes and point out areas of further growth. The PEER™ will systematize this process, underscoring excellence, and pointing out areas for improvement rather than credentialing.
The second product that will emerge out of our partnership with Metacred is a credentialing process for our external providers. Our first goal here is a review process for external treatment providers that certifies they have expertise in the myriad skills needed to ensure the best long-term outcome for our participants.11 Preliminary discussion of this certification with treatment providers has been very positive. They are excited about being recognized for the specialized services they provide to healthcare professionals.
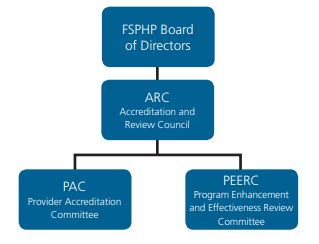
Figure 1
The FSPHP Board has approved a governance and oversight structure for this entire process. FSPHP members, the Metacred team, and select external experts will work on the structure and execution of these two review processes. The Program Enhancement and Effectiveness Review Committee (PEERC™) is charged with the construction, execution, and oversight of the PEER™ process. The Provider Accreditation Committee (PAC) will do the same for the provider credentialing process. These two committees will report to the Accreditation and Review Council (ARC), who will ensure a smooth implementation process faithful to the overarching goals of the FSPHP itself. The ARC will in turn report to the Board (see Figure 1).
Needless to say, formalizing the process of PHPs and their providers is a huge and rather expensive endeavor. I am happy to report that, thanks to the tireless efforts of our Executive Director, Linda Bresnahan, we have already received donations from organized medicine for half of the initial expenses for this project. The quantity and size of these donations tell us two things: One, medicine believes in us and what we do and two, organized medicine is telling us this should be done.
The FSPHP is on a wild ride, a growth spurt that deepens our commitment to the health of healers across North America. Welcome aboard!
References
1Mason, Dave. World in Changes, released 1970.
2Urban, Tim. The AI Revolution: The Road to Superintelligence, https:// waitbutwhy.com/2015/01/artificial-intelligence-revolution-1.html. 3Accenture Staff. The (Independent) Doctor Will NOT See You Now. White paper, available at: https://www.accenture.com/ t20150608T044420__w__/us-en/_acnmedia/Accenture/ Conversion-Assets/DotCom/Documents/Global/PDF/Dualpub_15/ Accenture-The-Doctor-Will-Not-See-You.pdf.
4Pallardy, C. 2015 Independent Physician Outlook: Nine Key Points, https://www.beckersasc.com/asc-turnarounds-ideas-to-improve -performance/2015-independent-physician-outlook-9-key-points.html.
5Gabbard, G. O. (1985). “The role of compulsiveness in the normal physician.” JAMA 254(20): 2926–2929.
6Maslach, C., & Jackson, S. E. (1981). “The measurement of experienced burnout.” Journal of Occupational Behavior, 2, 99–113.
7Schernhammer, E. S., & Colditz, G. A. (2004). Suicide rates among physicians: a quantitative and gender assessment (meta-analysis). American Journal of Psychiatry, 161(12): 2295–2302.
8Johns Hopkins Medical Institutions. “Physicians’ Divorce Risk May Be Linked to Specialty Choice.” ScienceDaily, 13 March 1997.
9FSPHP (2005). “FSPHP Physician Health Program Guidelines,” 2016, from https://www.fsphp.org/sites/default/files/pdfs/2005_ fsphp_guidelines-master_0.pdf.
10Metacred, About us, http://metacred.com/about-us. Accessed 31 July 2018.
11Earley, P. H. (2013). Safety Sensitive Workers. The ASAM Criteria: Treatment Criteria for Addictive, Substance-related and Co-occurring Disorders. Ed. D. Mee-Lee. Carson City, Nevada, The Change Companies: 460–483.
|